Picture in your mind a forty year old woman in her prime standing tall and proud before a crowd to receive an award. Now picture the same woman forty years later. She hobbles around, hunched over a cane and barely able to speak since she had her last stroke. What caused the gradual thinning of her bones and thickening of her arteries? Why does she have kidney stones, bone spurs and painful, swollen joints? What could she have done to prevent all this misery? One of the defining benchmarks of the aging process is the progressive movement of calcium and other minerals out of the bone (demineralization) and into the soft tissues of the body (calcification). Before we can understand the link between weak bones and aging, osteoporosis, cardiovascular disease, diabetes, hormonal imbalances and a host of other ailments, we need to first understand the critical roles our bones play in our health:
- Our bones provide structural support to protect inner organs and to act as a series of lever arms needed for movement.
- Our bones act as a factory for the production of blood products and a nursery for the maturation of immune cells.
- Our bones are a living and readily accessible storage depot of life-giving minerals that play a major role in regulating our body systems.
When you look at a skeleton you get the impression that bones are hard, solid and static or unchanging (in fact the word skeleton comes from the Greek word "skeletos", meaning "dried up"). Nothing could be further from the truth. Bones are indeed the second hardest substance in the human body (enamel is hardest), but they are neither solid nor static. Their internal structure is more like a honeycomb - a solid matrix (of protein, collagen and minerals) dotted with small holes. The minerals provide rigidity to the bone matrix while the protein and collagen provide some flexibility. Bones typically become more brittle as we age due to a loss of bone density as the bone matrix is progressively depleted of minerals. However, as we shall see, this does not have to be the case.
Osteoporosis - A modern epidemic
The World Health Organization defines osteoporosis as extremely low bone density - 2.5 standard deviations (SD) below "normal", which they set as the average peak bone mass of healthy young white women. In 1994 a new "precursor" condition of osteopenia (1-2.5 SD below normal) was introduced. According to the WHO definition, more than 70% of all women over age 50 have either osteoporosis or osteopenia. The National Osteoporosis Foundation's 2005 Annual Report calls osteoporosis a "major public health threat for an estimated 44 million Americans, or 55 percent of the people 50 years of age or older." It is a "silent disease" that progresses without any outward sign until a sufferer has a fracture.
This is a national health crisis that is not going away soon. In fact, the problem is growing exponentially as the baby boomer generation enters its golden years. The good news is that osteoporosis is absolutely preventable and to some extent reversible, but only if one is willing to learn how to eliminate those activities and foods that contribute to bone loss. More good news: eliminating those foods and activities will also greatly reduce your chances of developing a host of degenerative illnesses, especially if you supplement your diet with appropriate bone building nutrients in the correct proportions.
How and why does bone loss happen?
Skeletons may conjure up images of death, but our 206 bones are in fact living organs. Once they stop growing in size, they undergo constant repair and maintenance in a process known as remodeling. Remodeling is a two-part process. In part one (resorption), specialized cells called osteoclasts seek out bone tissue that has become weak or damaged and secrete an acid that dissolves the bone matrix, releasing calcium, magnesium and other minerals into the blood. In part two (mineralization), osteoblasts deposit new minerals and collagen into the areas that have been cleared. This is a much slower process, taking three to 18 months to complete, depending on one's age.
Early in life, mineralization outpaces resorption and our bones grow fast and strong, but then we enter a period where they are relatively equal (peak bone mass - twenties to early thirties) and eventually (if we do not choose to intervene with appropriate supplementation) inevitable and progressive bone loss sets in. Unfortunately for women, bone loss accelerates in the years surrounding menopause from a typical 1% to as much as 5% a year, so that the aforementioned elderly woman might have only 50% of her peak bone mass left. Not only is she at increased risk of heart disease and hip and other fractures, but depleted mineral stores along with her poor diet and failing digestion have greatly accelerated the aging process.
Bones are much more than a storage depot!
Bone remodeling is precisely controlled by hormones secreted by glands that directly or indirectly influence the major homeostatic control mechanisms in the body. Parathyroid hormone (PTH) is secreted by the parathyroid gland and stimulates osteoclasts to pull calcium from bones, while calcitonin (CT) is secreted by the thyroid gland and stimulates osteoblasts to deposit calcium into bones.
Remodeling is a critical feature of our incredible design in terms of our ability to regulate bodily functions such as blood pH, heart rate, and blood pressure in response to environmental and dietary changes. The bones act as an on demand storehouse of alkaline minerals which are accessed as needed to neutralize acid wastes, activate enzyme systems, and to regulate muscle contractions, blood clotting and nerve signaling.
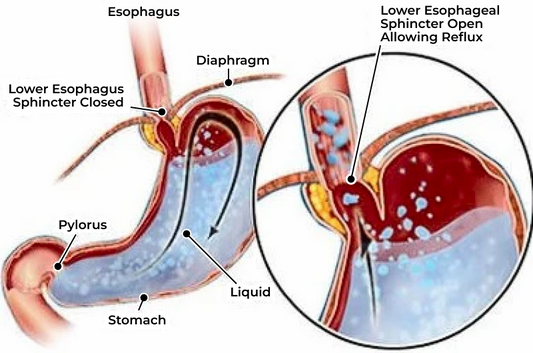
This is why pharmaceutical solutions to bone loss (an estimated six billion dollar market) such as bisphosphonates (i.e.- Fosamax, Actonel) are so insidious. Anti-resorption drugs may temporarily slow bone loss by shutting down osteoclast activity, but the critical health regulating aspects of bone remodeling are forfeited in the process (not to mention bone maintenance and integrity or the host of nasty side effects from gastric reflux to osteonecrosis of the jaw, a condition in which part or all of the jawbone dies). Parathryoid drugs (i.e.- Teraparatide) can stimulate bone growth, but they may also produce some severe side effects, from hypercalcemia to osteosarcoma (bone cancer).
Measuring Bone Loss
Proponents of bone density testing claim that DEXA machines are the gold standard for measuring bone health, but questions persist as to their validity. The problem is that no national or international standard for measuring peak bone mass has been accepted to date, and readings vary widely from brand to brand, making comparisons of different test results meaningless. Furthermore, bone mass varies with age, ethnicity, country (and even regions within countries), diet, and season - it is lower in the winter than in summer.
Predicting Fracture
Risk Along with expensive and dangerous drugs, bone mineral density (BMD) testing has been heavily promoted as a means to predict and prevent fractures. However, as a 1997 review by the British Columbia Health Technology Assessment Agency states, "Even the most favorable reports on the effectiveness of BMD testing reveal that low bone density alone does not accurately identify women who will go on to fracture as they age."
Accurately predicting fracture risk requires that many other factors are considered, including family history, diet and lifestyle issues, and especially body weight. It turns out that putting on those few extra pounds on the hips gives women a protective effect from fractures in two ways:
1) Even if they don't exercise, their bones are getting more resistance and thus respond by conserving bone mass.
2) Their fat cells produce estrogen, which has a bone sparing effect. According to a recent NIH report, 80% of women aged 75 or older would rather die than experience a hip fracture that lands them in a nursing home. Other Factors in Bone Loss Bone loss is certainly a natural part of the aging process, but in addition to genetics, there are a number of other lifestyle and dietary factors that can lead to intensified bone loss:
- Even moderate regular intake of caffeine (from coffee, tea, sodas or chocolate) had been shown to double the risk of hip fracture. Excessive alcohol consumption reduces bone density by suppressing osteoblast activity.
- Alcoholism is also associated with poor nutrition and increased risk of falls and fractures.
- Smoking cigarettes also inhibits osteoblast activity and further reduces bone density by suppressing estrogen levels (estrogen has a sparing effect on bone).
- Excessive intake of refined sugar and flour leads to acidosis, a condition in which acid buildup in the body requires the sacrificing of bone to generate the alkalizing minerals necessary to neutralize acid wastes and maintain the slightly alkaline pH of the blood. Drinking sodas is one of the worst offending habits in terms of building up acids in the body. Inadequate digestion, whether from poor dietary choices or from the body's inability to absorb and assimilate key nutrients, leads to increased bone loss.
- Many elderly people lack sufficient acid levels in the stomach to break down proteins and thus develop mineral deficiencies, creating more demand on the bones for mineral supply.
- Prescription and OTC Drugs can have devastating effects on bone health. Corticosteroid drugs (i.e.? Prednisone) rapidly accelerate bone loss as do antacids, acid blockers and certain tranquilizers. Lack of exercise also accelerates bone loss. Moderate exercise is critical for maintaining or building bone mass because bones respond to the stress of resistance training by getting stronger.
Bone metabolism is also dramatically affected by levels of sex hormones and synergistic minerals such as zinc, manganese, copper, boron, silicon, strontium and by the availability of critical nutrients such as vitamins C, B-6 and especially D-3 and K-2 (which acts as the "glue" that binds calcium into the bone matrix). Vitamin D may be the one most important nutrient needed for bone building. According to researchers, if you are low on vitamin D, you absorb as much as 65% less calcium. By far the two most important of all the bone nourishing minerals are calcium and magnesium.
Calcium and Magnesium? Critical to Bone and Cardiovascular Health
Calcium and magnesium are synergistic minerals. They work together in delicate balance to control many aspects of healthy physiology. For example, calcium promotes muscle contraction while magnesium promotes muscle relaxation. Cramps are simply contracted muscles that lack sufficient magnesium to relax fully. Magnesium deficiency may compromise heart health by disrupting the orderly contraction and relaxation of the heart muscle. Similarly, too much calcium in relation to magnesium can promote constipation because the smooth muscles of the bowel contract normally but don't relax as they should, so the rhythmic movement of food through the bowel (peristalsis) is disturbed. Calcium is absorbed in the intestinal tract only to the degree that certain nutrients are available to bind and transport it into the blood stream.
Restoring Bone Mass: Its all in the Ratio!
The need for calcium and magnesium supplementation is well established today, but the majority of Cal/Mag products offer poorly absorbed inorganic mineral forms (typically calcium carbonate) presented in the wrong ratio (anywhere from 10:1 to 4:1). Many bone health formulations contain calcium only, and those that do contain some magnesium are heavily weighted toward calcium. The problem is that most Americans are magnesium deficient in the first place, and when we lack magnesium, the balance between PTH and calcitonin is shifted causing osteoclasts to mine calcium from the bones. Worldwide, the rate of osteoporosis is highest in nations with the highest calcium intake and high ratios of calcium to magnesium, so the solution is clearly not just taking more calcium.
What is needed to restore this mineral and hormone imbalance (and resulting bone loss) is not a typical Cal/Mag product, but a Mag/Cal supplement (emphasizing magnesium over calcium) that also contains all the synergistic bone minerals and nutrients. Such a product may not only help restore bone mass, preserving the body's vital storehouse of minerals, but it may have profound implications in cardiovascular health, brain health, blood sugar metabolism and in slowing the aging process in general.
Long term consumption of excessive calcium (especially in relation to magnesium) can actually promote leaching of calcium from the bones and lead to a buildup in the urinary tract, gall bladder (kidney and gall stones), arteries or other internal organs - even the brain. Rather than introducing massive quantities of poorly absorbed calcium into the body in hopes of it being assimilated and properly excreted (which is what modern and even much of alternative medicine is doing), wouldn't it make more sense to target and restore calcium metabolism itself?
A More Desirable Outcome
What if the forty year old woman we began with made different choices (such as a wholesome diet and regular exercise) that did not set in motion changes that accelerate aging and bone loss? What if she chose to supplement her diet with highly absorbed forms of magnesium and calcium (along with other critical bone building nutrients) in appropriate proportions instead of harmful synthetic chemicals that manipulate her metabolism and add insult to injury? Perhaps then her golden years would not be plagued with misery and she would be healthy and productive all her days. For her sake and for the sake of her loved ones, I sure hope that she is reading this, because her answer is here MagnifiCal .
References
Reprinted with the permission of the World Health News
1. Effect on bone and mineral metabolism in the mouse. Calcif. Tissue Int., 2003, 72, pp32-41
2.Fuchs, NK.. Magnesium: A key to calcium absorption. The magnesium website. Nov. 2002
3.Journal of Reproductive Medicine. 1999;35:503
4. Sojka, J.E. Weaver, C.M. Nutrition Review. 1995, March: 53 (3). Pp. 71-74
5. National Health and Nutrition Examination Survey. NHANES 111, 1988-1991
6.Continuing Survey of Food Intakes of Individuals. CSFII, 1994 7. The Acid Alkaline Food Guide, Susan E. Brown, PhD (Square One Publishers), 2006.